Has that “cotton mouth” feeling become an all-too-familiar part of your day? Do you find yourself constantly reaching for water, struggling to eat certain foods, or even noticing changes in your breath? You’re not alone. The discomfort of dry mouth, medically known as xerostomia, is more than just an annoyance; it’s a silent alarm bell for your oral health, profoundly impacting the intricate world within your mouth. But what if the solution to a healthier, more comfortable mouth wasn’t just about sipping more water or using a special rinse? What if it started with what’s on your plate? For years, we’ve focused on hydration as the primary defense against dry mouth. And while crucial, it’s just one piece of a much larger puzzle. Today, we’re going to dive into a fascinating, often overlooked connection: how your dietary choices profoundly influence your oral microbiome – the bustling community of bacteria in your mouth – and how this delicate balance holds the key to managing dry mouth and protecting your smile.
Get ready for some “aha moments” that will change how you think about your next meal.
What Exactly Is Dry Mouth (Xerostomia)?
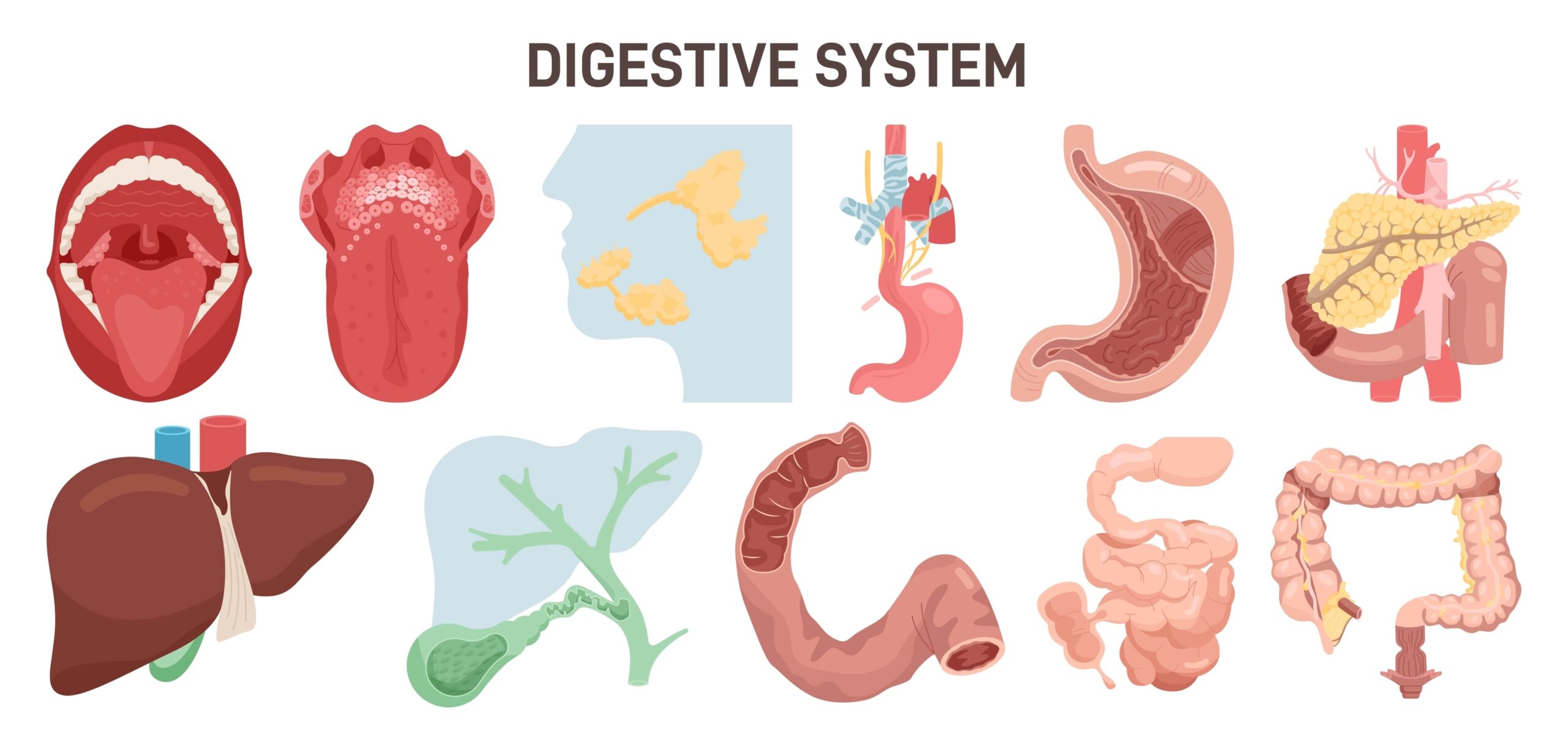
Imagine your mouth is a beautiful, self-cleaning ecosystem, and saliva is its lifeblood. Xerostomia occurs when your salivary glands don’t produce enough saliva, or when the saliva produced isn’t as effective.
This isn’t just about feeling parched; it’s about losing a vital bodyguard for your oral health.
Common culprits include:
- Medications: Over 500 prescription and over-the-counter drugs list dry mouth as a side effect, including those for allergies, depression, high blood pressure, and pain.
- Medical Conditions: Autoimmune diseases like Sjögren’s syndrome, diabetes, Parkinson’s disease, and even anxiety can significantly reduce saliva flow.
- Cancer Treatment: Radiation therapy to the head and neck, and certain chemotherapy drugs, can damage salivary glands.
- Lifestyle Factors: Smoking, alcohol consumption, and chronic dehydration also play a role.
- Nerve Damage: Injury to the head or neck can sometimes affect the nerves that signal salivary glands.
Without enough saliva, your mouth loses its natural ability to cleanse, neutralize acids, and protect against harmful bacteria.
The Unsung Hero: Why Saliva Matters So Much
Think of saliva as your mouth’s unsung hero, constantly working behind the scenes.
It’s not just water; it’s a complex fluid packed with enzymes, minerals, and antibodies, performing multiple critical jobs:
- Cleansing: It washes away food particles and debris, preventing them from sticking to your teeth and gums.
- pH Buffering: Saliva neutralizes acids produced by bacteria after you eat or drink, protecting your tooth enamel from erosion.
- Remineralization: It delivers essential minerals like calcium and phosphate back to your tooth surfaces, helping to repair early enamel damage.
- Antimicrobial Action: Saliva contains special proteins and enzymes that fight off harmful bacteria, viruses, and fungi.
- Digestion: It initiates the digestive process, breaking down food and making it easier to swallow.
- Speech & Taste: Without it, talking becomes difficult, and your sense of taste is diminished.
When this hero is missing in action, the stage is set for a dramatic shift in your mouth’s delicate balance.
Your Mouth’s Secret Garden: The Oral Microbiome
Beneath the surface of your tongue, gums, and teeth lies a bustling metropolis: your oral microbiome.
This “secret garden” is home to billions of bacteria, viruses, and fungi – a diverse community of over 700 species. Don’t worry, most of them are beneficial or harmless!
Think of it like a thriving garden:
- Beneficial Bacteria: These are the healthy plants and friendly insects that keep the garden vibrant. They help digest food, protect against invaders, and maintain a balanced ecosystem.
- Harmful Bacteria: These are like weeds or pests. In a healthy garden, they’re kept in check by the good guys.
- Balance (Eubiosis): A healthy oral microbiome has a diverse population, where beneficial species outnumber or control the harmful ones.
- Imbalance (Dysbiosis): When the “weeds” take over, or the “friendly plants” start to die off, the garden becomes unhealthy.
This balance is crucial because it’s your first line of defense against disease.
The Vicious Cycle: How Dry Mouth Wrecks Your Oral Microbiome
Now, let’s bring it back to dry mouth. When saliva flow diminishes, that vital “river” that irrigates your oral garden starts to dry up.

This creates an environment where the “weeds” – harmful, acid-producing bacteria like Streptococcus mutans – thrive.
Here’s how the vicious cycle unfolds:
- Loss of Cleansing: Food particles and sugars linger longer on tooth surfaces, providing a feast for cavity-causing bacteria.
- Loss of pH Buffering: The acidity in your mouth increases rapidly after meals and stays high, constantly eroding enamel.
- Reduced Antimicrobial Action: The protective enzymes and antibodies in saliva are gone, leaving your mouth vulnerable to bacterial and fungal overgrowth, like thrush.
- Shift in Bacteria: The lack of moisture and pH changes favor the growth of pathogenic bacteria, leading to oral dysbiosis. Beneficial bacteria struggle to survive.
This imbalance is a significant factor in why individuals with xerostomia often experience a dramatic increase in issues like:
- Cavities: The primary defense against tooth decay is compromised, leading to rapid development of [cavities].
- Gum Disease (Gingivitis and Periodontitis): Harmful bacteria proliferate, causing inflammation and infection of the gums.
- Oral Thrush: A fungal infection that appears as white patches.
- Bad Breath (Halitosis): Caused by the breakdown products of opportunistic bacteria.
- Difficulty Eating and Swallowing: Leading to poor nutrition.
Beyond Hydration: How Diet Becomes Your Oral Microbiome’s Best Friend
Here’s the exciting part: you have a powerful tool to interrupt this vicious cycle and nourish your oral ecosystem – your diet! It’s not just about what you avoid, but what you embrace.
By making targeted dietary choices, you can actively promote a balanced microbiome, support saliva production, and build a more resilient mouth.
Think of your food as fertilizer for your oral garden. We need to feed the good bacteria and starve the bad ones.
Dietary Superheroes for Your Dry Mouth & Microbiome:
Hydration Heroes (Beyond Plain Water):
While sipping water throughout the day is crucial, some foods and drinks offer a supercharged hydrating effect and even stimulate saliva production.
- Water-Rich Fruits & Vegetables: Cucumbers, watermelon, berries, celery, spinach, lettuce. These foods not only hydrate but often require chewing, which naturally stimulates saliva.
- Soups & Broths: Warm, clear broths can be incredibly soothing and hydrating.
- Herbal Teas: Non-caffeinated options like chamomile or ginger tea can provide moisture and comfort. Avoid adding sugar.
Prebiotics: Fuel for Your Good Bacteria:
Prebiotics are non-digestible fibers that act as food for beneficial bacteria, helping them grow and thrive. Just like gut bacteria, your oral good guys love them!
- Whole Grains: Oats, barley, brown rice.
- Legumes: Lentils, chickpeas, beans.
- Certain Fruits & Vegetables: Bananas, apples (with skin), onions, garlic, asparagus.
- Why they work: These foods encourage the growth of beneficial bacteria that produce short-chain fatty acids, which can help maintain a healthy oral pH and inhibit the growth of pathogens.
Probiotics: Friendly Forces for Your Mouth:
Introducing beneficial bacteria directly into your mouth can help restore balance.
- Sugar-Free Yogurt & Kefir: Look for live and active cultures.
- Fermented Vegetables: Kimchi, sauerkraut (rinse them if they’re very acidic or salty to protect enamel, especially with dry mouth).
- Specific Oral Probiotics: Some lozenges or chewing gums contain specific strains like Lactobacillus reuteri or Streptococcus salivarius K12, which have been shown to colonize the mouth and outcompete harmful bacteria.
Healthy Fats & Proteins:

These components can help cushion your teeth and oral tissues from acidic attacks and are essential for overall tissue repair.
- Lean Proteins: Chicken, fish, tofu, eggs.
- Healthy Fats: Avocados, nuts, seeds, olive oil.
- Why they work: They don’t ferment into acid like carbohydrates, and some fats can even coat teeth, offering a temporary protective barrier.
Vitamins & Minerals for Oral Health:
Certain micronutrients play a direct role in saliva production, tissue health, and immune function.
- Vitamin A: Essential for healthy mucous membranes (which line your mouth). Found in carrots, sweet potatoes, spinach.
- B Vitamins: Particularly B2, B3, B6, and B12, are crucial for cell health and can impact salivary gland function. Found in leafy greens, whole grains, lean meats.
- Zinc: Supports the immune system and can aid in wound healing. Found in nuts, seeds, legumes, meat.
Foods & Habits to Rethink (and Why):
Just as you nourish the good, it’s equally important to limit what fuels the bad.
- Sugary & Acidic Foods/Drinks: This is the big one. Candies, sodas, fruit juices, sports drinks, and even dried fruit provide a direct energy source for acid-producing bacteria, plummeting your mouth’s pH and supercharging tooth decay. With dry mouth, your saliva can’t buffer these acids effectively, making the damage far worse.
- Dry, Crumbly, Sticky Foods: Crackers, chips, certain breads, and peanut butter can be incredibly difficult to swallow without adequate saliva, and their small particles can cling to teeth, becoming a bacterial buffet.
- Caffeine & Alcohol: Both are diuretics, meaning they increase urine production and can contribute to overall dehydration, worsening dry mouth symptoms. Limit coffee, tea, and alcoholic beverages.
- Smoking/Vaping: Tobacco products are notorious for exacerbating dry mouth and significantly increasing the risk of oral health problems.
- Alcohol-Based Mouthwashes: While they may promise freshness, many commercial mouthwashes contain alcohol, which can further dry out and irritate already sensitive oral tissues. Opt for alcohol-free alternatives or a simple saline rinse.
Crafting Your Oral Microbiome-Friendly Meal Plan (Example)
Here’s a snapshot of how you might integrate these principles into a day:
- Breakfast: Oatmeal with fresh berries (prebiotics, hydration), a scoop of sugar-free Greek yogurt (probiotics), and a handful of almonds (healthy fats).
- Lunch: A large salad with mixed greens, cucumber, carrots, chickpeas (prebiotics, hydration), grilled chicken or tofu (protein), and an olive oil vinaigrette (healthy fats).
- Snack: Apple slices (prebiotics, hydration) with a smear of natural, sugar-free peanut butter (protein, healthy fats).
- Dinner: Baked salmon (protein, healthy fats) with steamed asparagus (prebiotics) and brown rice (prebiotics).
- Throughout the Day: Sip water constantly. Consider an unsweetened herbal tea. Chew sugar-free gum with xylitol (stimulates saliva).
Addressing Common Misconceptions Related to Dry Mouth:
- “All mouthwash is good for dry mouth.”
Truth: Many commercial mouthwashes contain alcohol, which can further dry and irritate your mouth. Always choose alcohol-free options specifically designed for dry mouth, or simply use a saline rinse.
- “Drinking more water is always enough to fix dry mouth.”
Truth: While essential, water alone often isn’t enough, especially if salivary glands are compromised. Diet and professional dental care are crucial for managing the root causes and preventing complications like rampant decay.
- “Dry mouth is just a normal part of aging.”
Truth: While older adults are more likely to take medications that cause dry mouth, xerostomia itself is not a normal part of healthy aging. It’s a symptom that warrants and treatment.
The Oral-Gut Axis: A Whole-Body Connection
The intricate dance of bacteria in your mouth doesn’t stay confined to your oral cavity.
Emerging research highlights the “oral-gut axis,” demonstrating that the health of your oral microbiome can directly influence your gut microbiome, and vice versa.
An imbalanced oral microbiome can mean harmful bacteria travel to your gut, potentially contributing to digestive issues and systemic inflammation.
By nurturing your oral garden through diet, you’re not just supporting your mouth; you’re contributing to your overall well-being.
When to Call in the Experts
While dietary changes are a powerful and proactive step, they are part of a comprehensive management plan.
If you’re experiencing persistent dry mouth, it’s crucial to consult with a dental professional like [Dr. Seema Shetty] and your general physician. They can help:
- Identify the Cause: Review your medications, medical history, and conduct necessary tests.
- Recommend Solutions: Prescribe saliva-stimulating medications, recommend specific oral hygiene products, or suggest artificial saliva substitutes.
- Address Complications: Treat cavities, gum disease, or oral infections that have arisen due to dry mouth.
- Provide Personalized Guidance: Offer tailored advice for your unique situation, integrating dietary changes with other treatments to protect your smile and health. Regular [professional dental care] is more important than ever with dry mouth.
Your Journey to a Healthier Smile Starts Now
The journey to managing dry mouth effectively is a marathon, not a sprint.
But by understanding the profound connection between your diet and your oral microbiome, you now hold the power to cultivate a healthier, more comfortable mouth.
Embrace water-rich foods, fuel your good bacteria with prebiotics and probiotics, and be mindful of what truly harms your oral ecosystem.
These seemingly small dietary shifts can lead to significant improvements in comfort, breath, and your long-term oral health. Your mouth’s secret garden will thank you.
Frequently Asked Questions (FAQ)
Q: Can dry mouth ever be cured?
A: It depends on the cause. If dry mouth is due to a reversible cause (e.g., a medication that can be changed, or dehydration), it might be fully resolved. If it’s due to a chronic condition or irreversible salivary gland damage, it’s often a chronic condition that needs ongoing management rather than a “cure,” but symptoms can be significantly improved.
Q: How quickly will I see results from dietary changes?
A: You might notice some immediate comfort from increased hydration and avoiding irritants. However, measurable shifts in your oral microbiome and a reduction in associated issues like cavities may take several weeks to months of consistent dietary changes combined with good oral hygiene.
Q: Are artificial saliva products effective?
A: Yes, artificial saliva substitutes (gels, sprays, rinses) can provide temporary relief from dry mouth symptoms by lubricating the mouth. They are a great tool for immediate comfort but don’t address the underlying cause or restore the full protective functions of natural saliva.
Q: What if my dry mouth is caused by medication?
A: If medication is the cause, speak to your doctor about potential alternatives or dosage adjustments. Never stop medication without medical advice. Your dentist can also provide strategies to manage the symptoms and protect your oral health while you continue necessary medications.
Q: Is xylitol really helpful?
A: Absolutely! Xylitol is a natural sugar alcohol found in many plants. It cannot be metabolized by Streptococcus mutans, the primary cavity-causing bacteria. In fact, it inhibits their growth and reduces acid production. Chewing sugar-free gum with xylitol can also stimulate saliva flow, making it a double win for dry mouth sufferers.
Ready to Learn More? Explore Our Resources!
Understanding your oral health is the first step toward a lifetime of confident smiles. If you have questions about dry mouth, your oral microbiome, or any other dental concerns, don’t hesitate to reach out. Your journey to a healthier mouth is a partnership, and we’re here to help guide you every step of the way.