Ever woken up with a sore jaw, a parched mouth, or a nagging headache, wondering where they came from? What if these seemingly disconnected discomforts were actually whispering a secret about your overall health – a secret deeply tied to how you breathe when you sleep? Many of us brush off snoring as a quirky habit or occasional teeth grinding as a stress response. But for a surprising number of people, these aren’t isolated incidents. They’re often interconnected dots on a critical map we call The Oral Health Cascade. This cascade illustrates how issues like snoring and sleep apnea can set off a chain reaction, leading to conditions such as persistent dry mouth, severe teeth grinding (bruxism), and uncomfortable temporomandibular joint (TMJ) issues.
At Smile Makers Dental Care, we believe that understanding these connections is the first step toward better health. Let’s explore this fascinating, yet often overlooked, relationship.
Unpacking the Foundation: Your Sleep and Your Mouth
Before we dive into the cascade, let’s get a clear picture of the key players involved.
Sleep-Disordered Breathing: More Than Just Snoring
When we talk about sleep-disordered breathing (SDB), we’re referring to a spectrum of conditions where your breathing isn’t smooth or consistent during sleep.
- Snoring: This familiar rumble occurs when air struggles to flow freely through your airway, causing tissues in your throat to vibrate. While often harmless, loud, habitual snoring can be a red flag.
- Sleep Apnea (Specifically Obstructive Sleep Apnea – OSA): This is a more serious condition where your airway repeatedly becomes completely or partially blocked during sleep, causing you to stop breathing for brief periods. Your brain, sensing the lack of oxygen, briefly wakes you up to restart breathing, often with a gasp or choke you might not even remember. This constant interruption means you never achieve truly restorative sleep.
The “Big Three” Oral Issues Triggered by Sleep
These are the common oral health problems often exacerbated or even caused by sleep-disordered breathing:
- Bruxism (Teeth Grinding or Clenching): You might do it subconsciously while awake, but nighttime bruxism is particularly damaging. It involves forcefully clenching your jaws or grinding your teeth together, often without your awareness until symptoms appear.
- Dry Mouth (Xerostomia): This isn’t just about feeling thirsty; it’s a chronic lack of saliva, which is vital for neutralizing acids, washing away food particles, and protecting your teeth.
- TMJ Discomfort (Temporomandibular Joint Disorder): The TMJ is the hinge connecting your jawbone to your skull. When it’s stressed or inflamed, it can lead to pain in your jaw, face, neck, and even clicking or locking of the jaw.
Lifestyle Factors: The Silent Influencers
It’s important to remember that our lifestyle choices don’t just affect our general well-being; they play a significant role in influencing sleep-disordered breathing and, consequently, our oral health.
Factors like excess weight, alcohol consumption (especially before bed), smoking, and even your sleep position can all contribute to or worsen snoring and sleep apnea.
Decoding the Oral Health Cascade: The Domino Effect
Now, let’s connect these dots and see how sleep-disordered breathing can set off a series of reactions that impact your oral health.
Think of it as a domino effect, where one problem leads directly to another.
Stage 1: Sleep-Disordered Breathing Triggers Oral Problems
- Obstructed Breathing Leads to Mouth Breathing: When your nose or throat airway is blocked, your body’s natural response, especially during sleep, is to open your mouth to get enough air. This is a crucial first step in the cascade.
- Mouth Breathing Causes Dry Mouth: Breathing through your mouth, particularly for extended periods at night, bypasses the natural humidifying function of your nose. This leads to increased evaporation of saliva, resulting in chronic dry mouth. Saliva is our mouth’s natural protector, full of minerals and enzymes that fight bacteria and neutralize acids. Without it, your mouth becomes a breeding ground for problems.
- Oxygen Deprivation Triggers Jaw Reflexes and Bruxism: This is one of the most significant “aha moments” for many. Research suggests that when your oxygen levels drop during sleep apnea episodes, your brain triggers a reflex in your jaw muscles. This reflex causes you to clench or grind your teeth, often unconsciously. Why? It’s your body’s frantic attempt to shift your jaw forward, open your airway, and restart breathing. In essence, your bruxism might not just be stress; it could be your body fighting for air.
Myth vs. Fact:
Myth: Snoring is harmless, just a noisy sleep habit.
Fact: While not all snoring indicates sleep apnea, loud, habitual snoring, especially if accompanied by gasping, choking, or daytime fatigue, is a significant warning sign of sleep-disordered breathing. Ignoring it can mean missing early indicators of the cascade.
The Vicious Cycle: When Oral Issues Fight Back
The cascade doesn’t stop there. Once dry mouth and bruxism take hold, they don’t just sit still; they exacerbate each other and lead to further, more severe oral health problems.
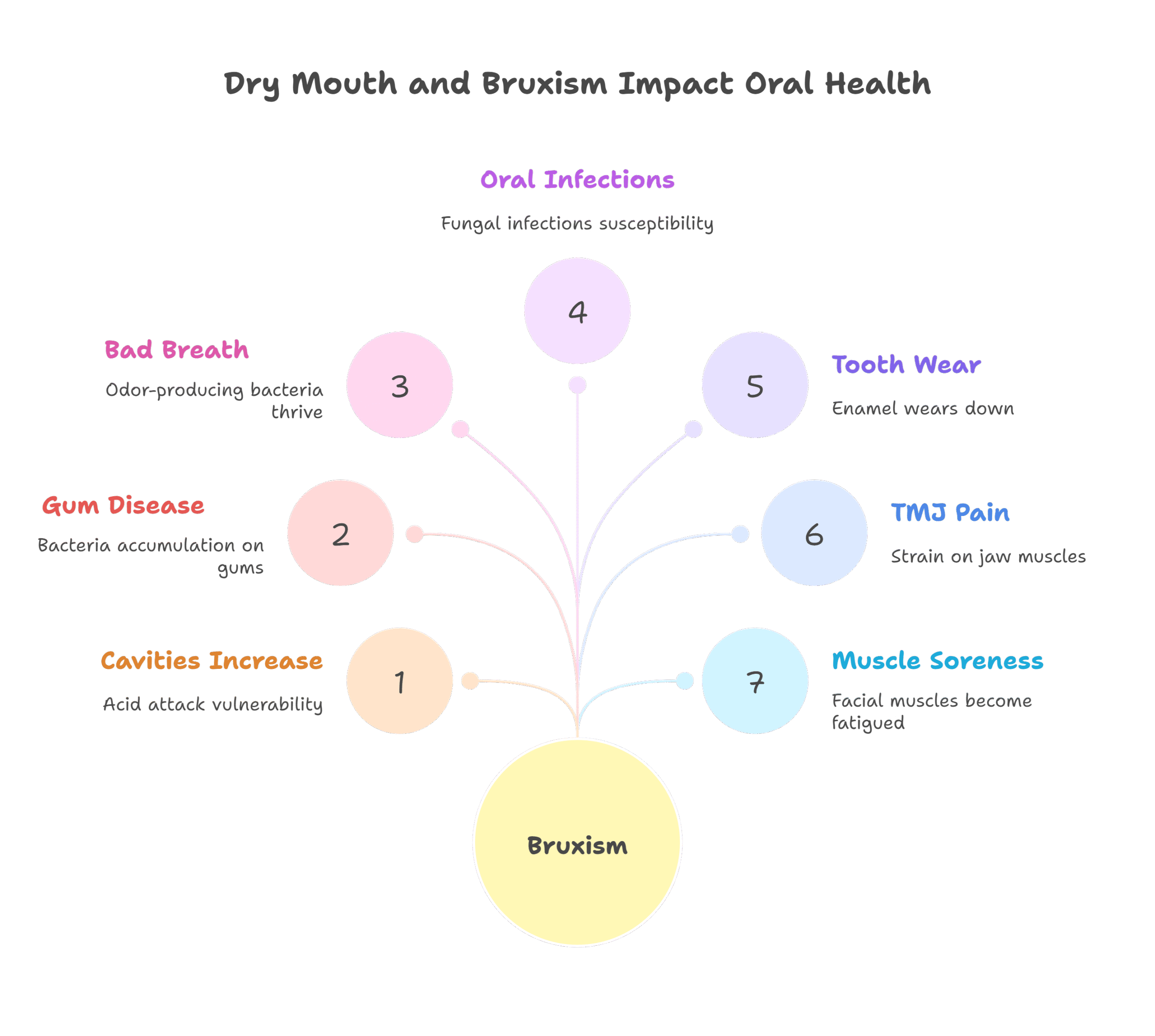
- Dry Mouth’s Domino Effect: Without adequate saliva, your mouth’s natural defense system collapses.
- Increased Cavities: Saliva helps wash away food particles and neutralizes plaque acids. Less saliva means more acid attacks and a higher risk of tooth decay, even if you brush regularly.
- Gum Disease: Dryness can lead to inflammation of the gums (gingivitis) and, if left untreated, progress to more serious periodontal disease, which can result in tooth loss.
- Bad Breath: Reduced saliva allows odor-producing bacteria to thrive.
- Oral Infections: Lack of saliva can make you more susceptible to fungal infections like oral thrush.
- Bruxism’s Long-Term Damage: The constant grinding and clenching exert enormous force on your teeth and jaw.
- Tooth Wear and Fractures: Over time, bruxism can flatten, chip, or crack your teeth. It can also wear down your tooth enamel, exposing the sensitive dentin underneath. In severe cases, it can damage existing dental work like crowns or fillings, sometimes even leading to the need for a Root Canal or Dental Implants.
- TMJ Pain and Headaches: The excessive strain on your jaw muscles and the TMJ can lead to chronic jaw pain, clicking or popping sounds, difficulty opening or closing your mouth, and tension headaches or migraines. [TMJ Therapy]
- Facial Muscle Soreness: Waking up with a tired or sore jaw is a classic sign of nighttime bruxism.
- How These Issues Worsen Sleep: It’s a cruel irony: the oral problems caused by poor sleep can, in turn, make your sleep quality even worse. Pain from bruxism or TMJ can disrupt sleep. Mouth breathing can lead to a less restorative sleep posture, and the cycle continues.
Spotting the Signs and Taking Action
Recognizing the signs of the oral health cascade is crucial for early intervention. You don’t have to wait for severe problems to develop.
Your Personal Cascade Checklist: Do You Have Any of These Symptoms?
- Do you wake up with a very dry mouth or sore throat?
- Is your tongue always dry, even after drinking water?
- Do you often experience morning headaches or jaw pain?
- Has your dentist noticed unusual tooth wear or cracks?
- Do you hear clicking or popping noises when you move your jaw?
- Has anyone told you that you snore loudly or gasp during sleep?
- Do you feel excessively tired during the day, even after a full night’s sleep?
If you answered yes to several of these, it’s a strong indicator that you might be experiencing the oral health cascade.
The Dentist’s Critical Role in Detection
Your dentist is often the first healthcare professional to spot the physical signs of this cascade.
During a routine dental checkup, Dr. Shetty and our team at Smile Makers Dental Care look for:
- Unusual tooth wear patterns
- Gum inflammation unrelated to oral hygiene
- Red, dry, or cracked oral tissues
- Signs of TMJ dysfunction
- Narrow dental arches or other anatomical features that could indicate airway issues
We can then guide you on the next steps, which often involve a consultation with a sleep specialist for a sleep study to diagnose sleep apnea or other sleep disorders. [about Dr. Seema Shetty]
Breaking the Cascade: Your Path to Better Health
The good news is that by understanding the cascade, you can take targeted steps to break its cycle and improve both your oral health and your overall well-being.
A multidisciplinary approach, often involving your dentist and a sleep physician, is most effective.
Addressing Sleep-Disordered Breathing
This is often the primary point of intervention, as it tackles the root cause.
- Lifestyle Changes:
- Weight Management: Losing even a small amount of weight can significantly improve sleep apnea symptoms.
- Avoid Alcohol and Sedatives: Especially before bed, as they relax throat muscles, worsening airway obstruction.
- Change Sleep Position: Sleeping on your side rather than your back can help keep your airway open.
- Quit Smoking: Smoking irritates and inflames the airway.
- Oral Appliance Therapy (OAT): Your dentist can custom-fit a removable [Oral Appliances] that you wear at night. These devices gently reposition your lower jaw and/or tongue forward, keeping your airway open and reducing snoring and mild to moderate sleep apnea.
- CPAP (Continuous Positive Airway Pressure): For more severe sleep apnea, a CPAP machine delivers a gentle stream of air through a mask worn during sleep, keeping the airway open.
- Surgical Options: In some cases, surgical procedures may be considered to remove excess tissue or reposition the jaw to open the airway.
Managing Oral Symptoms
While addressing the root cause, it’s also important to manage the existing oral damage.
- For Bruxism: Custom-fitted nightguards protect your teeth from the forces of grinding and clenching, preventing further wear and damage. Your dentist can also provide advice on stress management techniques.
- For Dry Mouth:
- Sip water frequently throughout the day.
- Use over-the-counter saliva substitutes (mouth sprays, gels, lozenges).
- Chew sugar-free gum to stimulate saliva flow.
- Use fluoride toothpaste and rinses to protect against cavities.
- Avoid caffeine, alcohol, and sugary drinks, which can worsen dryness.
- For TMJ Discomfort: Treatment may include custom oral appliances (splints), pain management, physical therapy, and lifestyle adjustments to reduce jaw strain.
- Restorative and Cosmetic Dentistry: Once the underlying issues are managed, damaged teeth can be repaired with [Fillings], crowns, or even [Cosmetic Dentistry] to restore their function and appearance.
Frequently Asked Questions About the Oral Health Cascade
Does snoring always mean I have sleep apnea?
Not necessarily, but loud, chronic snoring is a primary symptom of sleep apnea. Many people snore without having sleep apnea, but it’s important to be evaluated, especially if you experience daytime fatigue or witnessed breathing pauses. Your dentist or doctor can help you determine if further investigation is needed.
Can grinding my teeth really be linked to my breathing?
Yes, absolutely. As we discussed, a common theory suggests that during sleep apnea episodes, the body instinctively clenches or grinds its teeth in an attempt to open the airway and restart breathing. So, your bruxism could be a direct result of your body fighting for air.
Why is my mouth so dry in the morning, even if I drink water before bed?
Chronic dry mouth upon waking is a very common sign of mouth breathing during sleep. When you breathe through your mouth instead of your nose, especially for hours, saliva evaporates quickly, leaving your mouth parched. Sleep-disordered breathing can often lead to this mouth-breathing habit.
What’s the first step if I suspect I’m on this cascade path?
The best first step is to schedule a comprehensive dental exam. Your dentist is uniquely positioned to identify oral signs of sleep-disordered breathing and bruxism. They can discuss your symptoms, examine your oral cavity, and refer you to a sleep specialist if sleep apnea is suspected.
How common is this full cascade?
While specific statistics for the entire “oral health cascade” aren’t readily available, the prevalence of its individual components is high. For instance, sleep apnea affects millions, bruxism is widespread, and chronic dry mouth is a common complaint. Given the clear physiological links, it’s very common for individuals to experience multiple parts of this cascade, often without realizing the underlying connection.
Your Health Journey Starts Here
Understanding the Oral Health Cascade is a powerful step towards taking control of your health. It moves beyond treating isolated symptoms to recognizing the deep, interconnected relationship between your sleep and your oral well-being. If you suspect you’re experiencing any part of this cascade—whether it’s persistent dry mouth, jaw pain, or concerns about your snoring—don’t hesitate to reach out. At Smile Makers Dental Care in Brampton, Dr. Seema Shetty and our compassionate team are dedicated to helping you unravel these complexities.
We’re here to provide thorough evaluations, accurate diagnoses, and personalized care, guiding you toward a healthier, more comfortable future.